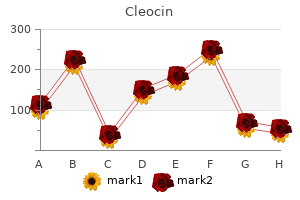
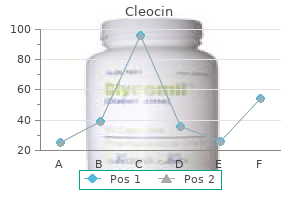
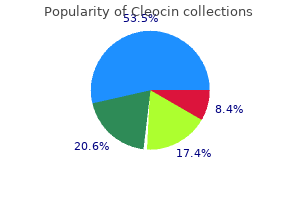
"150mg cleocin for sale, acne wallet".
By: D. Spike, M.B. B.CH., M.B.B.Ch., Ph.D.
Co-Director, University of New England College of Osteopathic Medicine
Myelitis Secondary to acne zits cysts and boils popped generic cleocin 150 mg online Bacterial acne 7dpo purchase cleocin discount, Fungal acne tool buy discount cleocin 150mg on-line, Parasitic, and Granulomatous Diseases With few exceptions, this class of spinal cord disease seldom offers any difficulty in diagnosis. In most cases, the inflammatory reaction in the meninges is only one manifestation of a generalized (systemic) disease process. The spinal lesion may involve primarily the pia-arachnoid (leptomeningitis), the dura (pachymeningitis), or the epidural space. In some acute forms, both the spinal cord and meninges are simultaneously affected, or the cord lesions may predominate. Chronic spinal meningitis may involve the pial arteries or veins; and as the inflamed vessels become thrombosed, infarction (myelomalacia) of the spinal cord results. Chronic meningeal inflammation may provoke a progressive constrictive pial fibrosis (socalled spinal arachnoiditis) that virtually strangulates the spinal cord. In certain instances, spinal roots become progressively damaged, especially the lumbosacral ones, which have a long meningeal exposure. Interestingly, there are cases of chronic cerebrospinal meningitis that remain entirely without symptoms until the spinal cord or roots become involved. The infrequent but unique bacterial myelitis caused by the atypical pneumonia agent Mycoplasma pneumoniae has come to be viewed as a postinfectious immune disease, as discussed on page 601. At times it stands as a single pyogenic metastasis, but more often there has been spread from a contiguous infected surgical site or a fistulous connection with a superficial paraspinal abscess or a distant infection and subsequent bacteremia. As stated, spinal epidural abscess and granuloma are the more important representatives of this group. Sarcoid myelitis (see also page 613) Sarcoid granulomas may present as one or more intramedullary spinal cord masses, as in the cases reported by Levivier and colleagues. In our experience the granulomatous lesion, which may be focal or multifocal, simulates demyelinative disease with respect to its tendency to relapse and remit and in its notable but inconsistent response to corticosteroids (page 614). An asymmetrical ascending paraparesis and bladder disturbance have been the main features in our patients. The most characteristic finding, however, is a multifocal-subpial nodular enhancement of the meninges adjacent to a lesion of the cord or nerve roots- a picture which to some extent resembles neoplastic meningeal infiltration. The diagnosis can be confirmed by mediastinal lymph node biopsy or by the less desirable method of biopsy of the spinal meninges and affected subpial cord. A number of other rare granulomatous conditions have on occasion caused an intrinsic or, more often, an extrinsic compressive myelopathy, including brucellosis, xanthogranulomatosis, and eosinophilic granuloma. The diagnosis may be suspected if the systemic disease is apparent at the time, but in some instances only the histology of a surgical specimen reveals the underlying process. Spinal Epidural Abscess this condition is worthy of emphasis because the diagnosis is often missed or mistaken for another disease, sometimes with disastrous results. Staphylococcus aureus is the most frequent etiologic agent, followed in frequency by streptococci, gram-negative bacilli, and anaerobic organisms. An injury to the back, often trivial at the time, furunculosis or other skin or wound infection, or a bacteremia may permit seeding of the spinal epidural space or of a vertebral body. This gives rise to osteomyelitis with extension of the purulent process to the epidural space. One frequent source is a septicemia in a drug addict following the use of nonsterile needles or the injection of contaminated drugs. In other cases organisms may be introduced into the epidural space during spinal surgery or rarely via a lumbar puncture needle during epidural or spinal anesthesia or from epidural injections of steroid or other therapeutic agents. In these cases of cauda equina epidural abscess, back pain may be severe and neurologic symptomatology minimal unless the infection extends upward to the upper lumbar and thoracic segments of the spinal cord. At first, the suppurative process is accompanied only by lowgrade fever and aching local back pain, usually intense, followed within a day or several days by radicular pain in most cases. Headache and nuchal rigidity are sometimes present; more often there is just the persistent pain and a disinclination to move the back. After several more days, there is the onset of a rapidly progressive paraparesis and paraplegia or quadriplegia associated with sensory loss in the lower parts of the body and sphincteric paralysis. Percussion of the spine elicits considerable tenderness over the site of the infection. Examination discloses all the signs of a complete or partial transverse cord lesion, occasionally with elements of spinal shock if paralysis has evolved rapidly, which is rare. The protein content is high (100 to 400 mg/100 mL or more), but the glucose is normal. Elevation of the sedimentation rate and peripheral neutrophilic leukocytosis are important clues (often neglected) to the diagnosis (Baker et al).
The tumors that arise from these cells are identical in appearance with tumors of other chemoreceptor organs (paragangliomas) acne kids purchase cleocin mastercard. Interestingly acne getting worse purchase 150mg cleocin with amex, they are 12 times more frequent in individuals living at high altitudes skin care brand crossword purchase cleocin online. Clinically the usual presentation is of a painless mass at the side of the neck below the angle of the jaw; thus it must be differentiated from the branchial cleft cyst, mixed tumor of the salivary gland, and carcinomas and aneurysms in this region. Tumors of the carotid body have been a source of transient ischemic attacks in 5 to 15 percent of the 600 or more reported cases. One of the most interesting presentations has been with sleep apnea, particularly with bilateral tumors (see below); respiratory depression as well as lability of blood pressure are common postoperative problems. A similar paraganglioma of the vagus nerve has been reported; it occurs typically in the jugular or nodose ganglion but may arise anywhere along the course of the nerve. These tumors may also undergo malignant transformation, metastasize, or invade the base of the skull. A carotid body tumor, separate in nature from the glomus jugulare tumor, has been seen in combination with von Recklinghausen neurofibromatosis. Familial cases are known, especially with bilateral carotid body tumors (about 5 percent of these tumors are bilateral). The treatment should be surgical excision with or without prior intravascular embolization; radiation therapy is not advised. Pituitary Adenomas (See also page 486) Tumors arising in the anterior pituitary are of considerable interest to neurologists because they often cause visual and other symptoms related to involvement of structures bordering upon the sella turcica before an endocrine disorder becomes apparent. Pituitary tumors are agelinked; they become increasingly numerous with each decade; by the 80th year, small adenomas are found in more than 20 percent of pituitary glands. On the basis of conventional hematoxylin-eosin staining methods, cells of the normal pituitary gland were for many years classified as chromophobe, acidophil, and basophil, these types being present in a ratio of 5:4:1. Adenomas of the pituitary are most often composed of chromophobe cells (4 to 20 times as common as acidophilcell adenomas); the incidence of basophil-cell adenomas is uncertain. Histologic study is now based on immunoperoxidase staining techniques that define the nature of the hormones within the pituitary cells-both of the normal gland and of pituitary adenomas. The development of sensitive (radioimmunoassay) methods for the measurement of pituitary hormones in the serum has made possible the detection of adenomas at an early stage of their development and the designation of several types of pituitary adenomas on the basis of the endocrine disturbance. Hormonal tests for the detection of pituitary adenomas, preferably carried out in an endocrine clinic, are listed in Table 31-3. Between 60 and 70 percent of tumors, in both men and women, are prolactin-secreting. These tumors may be monohormonal or plurihormonal and approximately one-third are composed of nonfunctional (null) cells. Pituitary tumors usually arise as discrete nodules in the anterior part of the gland (adenohypophysis). They are reddish gray, soft (almost gelatinous), and often partly cystic, with a rim of calcium in some instances. The adenomatous cells are arranged diffusely or in various patterns, with little stroma and few blood vessels; less frequently the architecture is sinusoidal or papillary in type. Tumors less than 1 cm in diameter are referred to as microadenomas and are at first confined to the sella. As the tumor grows, it first compresses the pituitary gland; then, as it extends upward and out of the sella, it compresses the optic chiasm; later, with continued growth, it may extend into the cavernous sinus, third ventricle, temporal lobes, or posterior fossa. Recognition of an adenoma when it is still confined to the sella is of considerable practical importance, since total removal of the tumor by transsphenoidal excision or some form of stereotactic radiosurgery is possible at this stage, with prevention of further damage to normal glandular structure and the optic chiasm. Penetration of the diaphragm sellae by the tumor and invasion of the surrounding structures make treatment more difficult. Pituitary adenomas come to medical attention because of endocrine or visual abnormalities. Headaches are present with nearly half of the macroadenomas but are not clearly part of the syndrome. The visual disorder usually proves to be a complete or partial bitemporal hemianopia, which has developed gradually and may not be evident to the patient (see the description of the chiasmatic syndromes on page 206). A small number of patients will be almost blind in one eye and have a temporal hemianopia in the other. This results in a central scotoma on one or both sides (junctional syndrome) in addition to the classic temporal field defect (see.
Somewhat fewer than 10 percent of patients have clinically evident neuropathy at the time of discovery of diabetes but this figure rises to skin care food generic cleocin 150 mg visa 50 percent after 25 years skin care yang terbaik discount cleocin 150mg overnight delivery. Dyck and colleagues (1993) studied 380 diabetics- 27 percent with type 1 (insulin-dependent) forms and 73 percent with type 2 (noninsulin-dependent); symptomatic polyneuropathy was found in 15 percent of the first group and 13 percent of the second acne rosacea order 150 mg cleocin with mastercard. The percentages were far higher when patients were selected electrophysiologically. Several fairly distinct clinical syndromes have been delineated: (1) the most common, a distal, symmetrical, primarily sensory polyneuropathy affecting feet and legs more than hands in a chronic, slowly progressive manner; (2) acute diabetic ophthalmoplegia that affects the third, and less often, the sixth cranial nerve; (3) acute mononeuropathy of limbs or trunk including a painful thoracolumbar radiculopathy; (4) a rapidly evolving, painful, asymmetrical, predominantly motor multiple neuropathy affecting the upper lumbar roots and the proximal leg muscles (socalled diabetic amyotrophy); (5) a more symmetrical, proximal motor weakness and wasting, often without pain and with variable sensory loss pursuing a subacute or chronic course; (6) an autonomic neuropathy involving bowel, bladder, and circulatory reflexes; and (7) a painful thoracoabdominal radiculopathy. These forms of neuropathy often coexist or overlap, particularly the autonomic and distal symmetrical types and the subacute proximal neuropathies. Most of the types of neuropathy listed above are thought to be due to ischemia or infarction of nerves or nerve fascicles, due to a diabetic microvasculopathy. The polyneuropathy is associated with small blood vessel disease (affecting the vaso nervorum) but possibly also with a poorly understood metabolic abnormality; however, other theories of causation abound. In recent years, an inflammatory process has been postulated as yet another mechanism of peripheral nerve damage. Distal Polyneuropathy the distal, symmetrical, primarily sensory form of polyneuropathy is the most common type. Although it is usually a chronic process, sometimes unnoticed by the patient, we include it here in order to provide a complete tabulation of the diabetic neuropathies. The main complaints are persistent and often distressing numbness and tingling, usually confined to the feet and lower legs, and worse at night. As a rule, sensory loss is confined to the distal parts of the lower extremities, but in severe cases the hands are involved and the sensory loss may even spread to the anterior trunk, giving rise to confusion in diagnosis (Said et al). Trophic changes in the form of deep ulcerations and neuropathic degeneration of the joints (Charcot joints) are encountered Diabetic Neuropathy Diabetes mellitus is the cause of the most common polyneuropathy in general clinical practice for which reason it is accorded a separate section. Several limited forms of peripheral nerve disease are also the direct result of diabetes and for convenience of exposition they are included here; some of these are acute and focal and enter into the differential diagnosis of mononeuritis multiplex considered in the next section. In another group of patients with diabetic polyneuropathy the clinical picture may be dominated instead by loss of deep sensation, ataxia, and atony of the bladder, with only slight weakness of the limbs, in which case it resembles tabes dorsalis (hence the term diabetic pseudotabes). The similarity is even closer if lancinating pains in the legs, unreactive pupils, and neuropathic arthropathy are present. Acute Diabetic Mononeuropathies Among these, diabetic ophthalmoplegia is a common occurrence, usually in a patient with well-established diabetes. It commonly presents as an isolated, painful third nerve palsy with sparing of pupillary function. In the first autopsied patient reported by Dreyfus, Adams, and colleagues, there was an ischemic lesion in the center of the retro-orbital portion of the third nerve. Isolated involvement of practically all the major peripheral nerves has been described in diabetes, but the ones most frequently involved are the femoral, sciatic, and peroneal nerves in about that order. As mentioned, the acute mononeuropathies, both cranial and peripheral, are presumably due to infarction of the nerve but it is in studies of the third nerve that this pathologic basis has been most convincingly established as noted above. Diabetic Multiple Mononeuropathies and Radiculopathies this category overlaps with the mononeuropathies. A syndrome of painful unilateral or asymmetrical multiple neuropathy tends to occur in older patients with relatively mild or even unrecognized diabetes. These affections of several single nerves occur in a random distribution and cause a mononeuritis multiplex. They often emerge during periods of transition in the diabetic illness, for example, when severe hyper- or hypoglycemia arises, when insulin treatment is being initiated or adjusted, or when there has been rapid weight loss. In the most characteristic type, which affects the lumbar roots, pain, which can be severe, begins in the low back or hip and spreads to the thigh and knee on one side. The discomfort has a deep, aching character with superimposed lancinating jabs, and there is a propensity for pain to be most severe at night. Weakness and later atrophy are evident in the pelvic girdle and thigh muscles, although the distal muscles of the leg may also be affected. Curiously, we have found the opposite patellar reflex to be absent in some patients. Deep and superficial sensation may be intact or mildly impaired, conforming to either a multiple nerve or multiple adjacent root distribution. Recovery is the rule although months and even years may elapse before it is complete.
Muscle relaxants are of little use acne needle purchase cleocin 150 mg, serving mainly to skin care coconut oil order 150 mg cleocin visa make bed rest more tolerable skin care yang bagus dan murah best order for cleocin. As a result of several studies that have failed to demonstrate a benefit of bed rest, recent practice has been to mobilize patients as soon as they are able and to prescribe corrective exercises designed to stretch and strengthen trunk (especially abdominal) muscles, overcome faulty posture, and increase the mobility of the spinal joints. Despite this modern approach, the authors can affirm from personal experience that some injuries produce such discomfort that arising from a bed or chair is simply not possible in the early days after injury. The use of spinal manipulation- practiced by chiropractors, osteopaths, and others- has always been a contentious matter in the United States, partly because of unrealistic therapeutic claims made in treating diseases other than low back derangements. By contrast, in certain parts of Europe, orthopedists often incorporate manipulative procedures into conventional practice. A type of slow muscle stretching and joint distraction (axial traction on a joint) administered by physiatrists and physical therapists is quite similar. It must be recognized that many patients seek chiropractic manipulation on their own, often before seeing a physician, and may not disclose this information to the physician. When the supporting elements of the spine (pedicles, facets, and ligaments) are not disrupted, chiropractic manipulation of the lumbar spine has provided acute relief to a considerable number of our patients with low back strain or facet pain; at issue is the durability of the effect, even with repeated so-called spinal adjustments. A randomized British trial has shown manipulation to be superior to analgesics and bed rest in returning patients to work after minor back injury (Meade et al). Some other trials have corroborated this finding (Hadler et al), while others have not, or, most often, the results have been ambiguous. In the study by Cherkin and colleagues comparing chiropractic, physical therapy (McKenzie method), and simple instruction to the patient from a booklet, manipulation yielded a slightly better outcome at the end of a month. Despite several hypotheses offered by practitioners of spinal manipulation, the mechanism of pain relief is not known. The sound created by rapid and forceful distraction of the facet joints, similar to cracking the knuckles, seems not to be necessary for pain relief. Whether all forms of low back pain represent minor subluxations, as claimed by chiropractors, is undocumented and seems unlikely. The results with another popular approach, acupuncture, have been even more uncertain for acute or chronic back pain, most studies showing it to be no more effective than a sham treatment (Tudler et al). The Degenerative Low Back Syndrome Often the symptoms of low back strain are recurrent and more chronic in nature, being regularly exacerbated by bending or lifting, suggesting that postural, muscular, and arthritic factors play a role. This is the most common syndrome seen in orthopedic clinics, more in men than in women. After some unusual activity, raising the question of trauma, especially if it happens in the workplace, the patient develops deep aching pain in the low back, increased by certain movements and attended by stiffness. The pain may additionally have a restricted radiation into the buttocks and posterior thigh, thereby simulating root compression. Plain films and imaging procedures reveal some combination of osteoarthropathy, changes in vertebral discs, osteoarthritic changes in apophysial joints, and sometimes osteoporosis or slight spondylosis. Treatment with short-duration bed rest, analgesics, and physiotherapy, as outlined for acute strains, helps to relieve the symptoms, and the majority of patients recover within a few weeks, only to have a recurrence of similar pains in the future. Recurrent attacks are typical of degenerative spine disease that affects the vertebrae and facet joints. Chiropractic manipulation has the same uncertain effect as for acute low back symptoms. Usually the origin of the pain cannot be determined and special diagnostic procedures are not helpful. Quite often, changing the stiffness of the mattress (in either direction) is helpful. Vertebral Fractures Fractures of lumbar vertebral bodies are usually the result of flexion injuries. Such trauma may occur in a fall or jump from a height (if the patient lands on his or her feet, the calcanei may also be fractured) or as a result of an auto accident or other violent injury. If the injury is severe, it may cause a fracture dislocation, a "burst" fracture of one or more vertebral bodies, or an asymmetrical fracture of a pedicle, lamina, or spinous process; most often, however, there is asymmetrical loss of height of a vertebral body (compression fracture), which may be extremely painful at the onset. When compression or other fractures occur with minimal trauma (or spontaneously), the bone has presumably been weakened by some pathologic process. Most of the time, particularly in older individuals, osteoporosis is the cause of such an event, but there are many other causes, including osteomalacia, hyperparathyroidism, prolonged use of corticosteroids, ankylosing spondylitis, myeloma, metastatic carcinoma, and a number of other local conditions. Spasm of the lower lumbar muscles, limitation of all movements of the lumbar section of the spine, and the radiographic appearance of the damaged lumbar portion (with or without neurologic abnormalities) are the basis of clinical diagnosis.
Order cleocin on line amex. My Evening Skin Care Routine.