"Cheap mentat ds syrup 100 ml online, medications gerd".
By: Z. Karlen, M.B. B.A.O., M.B.B.Ch., Ph.D.
Co-Director, Noorda College of Osteopathic Medicine
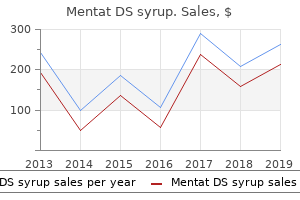
The volume of gas which can pass across the alveolar membrane per unit time at a given pressure is the diffusing capacity of the lungs treatment skin cancer purchase 100 ml mentat ds syrup with mastercard. The diffusing capacity is not only dependent on the difference in partial pressure of the gas in the alveolar air and pulmonary capillary blood medicine - discount mentat ds syrup amex, but it is also proportional to shinee symptoms order 100 ml mentat ds syrup mastercard such factors as the effective surface area of the pulmonary vascular bed. It is inversely proportional to the average thickness of the alveolar membrane and directly proportional to the solubility of the gas in the membrane. The normal values for diffusing capacity range from 20 to 30 ml 02/min/mm Hg for normal young adults. Underperfused or poorly ventilated alveoli can become a serious matter during flight when G forces acting on the body result in a redistribution of pulmonary capillary blood flow. During exposure to positive (+ Gz) accelerative forces, the blood flow is directed to the lung bases, whereas, during exposure to negative (- Gz) acceleration, the flow is toward apical areas. Composition of Respired Air the composition of the atmosphere is remarkably constant between sea level and an altitude of 300,000 feet. Nitrogen and oxygen are the most abundant gases in the atmosphere as shown in Table l-l. From a practical standpoint, in the study of the effects of altitude on the human body, the percent concentrations of the other gases are considered negligible and are ignored. It is convenient, therefore, to consider air as about four fifths (79 percent) nitrogen and one fifth (21 percent) oxygen. The water vapor has a constant pressure of 47 mm Hg at the normal body temperature of 98. Accordingly, the sum of the partial pressures of the inspired gases no longer equals the barometric pressure, but instead equals the barometric pressure minus the water vapor pressure. A constant, sea level ventilation rate and a normal metabolic rate are presumed for the sake of simplicity. Table l-6 shows measured changes at sea level in the partial pressure of the gases at various sites in the respiratory cycle. Physiology of Plight Table l-6 Partial Pressures of Respiratory Gases at Various Sites in Respiratory Circuit of Man at Rest at Sea Level Figure 1-3. Therefore, the capacity for 100 ml of blood is about 20 ml of oxygen (presuming normal hemoglobin to be 14. Normally, arterial hemoglobin in an individual breathing air at sea level is 98 percent saturated. When breathing 100 percent oxygen at sea level pressure, the hemoglobin becomes 100 percent saturated, and additional oxygen goes into simple solution in the plasma. From these curves it can be seen that the blood leaves the pulmonary capillary bed with the hemoglobin about 98 percent saturated. In the tissue capillaries, however, a small decrease in oxygen tension causes changes in the dissociation curve which result in a large quantity of oxygen being made available to the tissues. As the oxygen tension continues to fall, however, an additional reduction of 30 mm Hg results in a precipitous drop in blood saturation to 58 percent. Thus, the characteristic shape of the dissociation curves accounts for the relatively mild effects of hypoxia at low altitude and the very serious impairment of function at higher altitudes. The oxygen carrying capacity of the blood hemoglobin is also very sensitive to changes in blood pH (Bohr effect), as illustrated in Figure 1- 4B. Effect of acidity on oxygen dissociation curve of blood (after Peters & Van Slyke). Control of Respiration the neural control of respiration is accomplished by neurons in the reticular formation of the medulla. This rhythmic activity is modified by afferent impulses arising from receptors in various parts of the body, by impulses originating in higher centers of the central nervous system, and by specific local effects induced by changes in the chemical composition of the blood. However, if the afferent fibers from the chemoreceptive areas are severed, respiration is depressed. Even a reduction alveolar oxygen to about 40 mm Hg (42,000 feet equivalent altitude) will only increase ventilation by about one third of its normal resting value.
Diseases
- Hypertrophic branchial myopathy
- Anorexia nervosa binge-purge type
- Von Gierke disease
- Syndactyly cataract mental retardation
- Hereditary carnitine deficiency
- Hydrocephaly low insertion umbilicus
- Hypertrophic cardiomyopathy: familial
- Polymorphic macular degeneration
- Patel Bixler syndrome
- Cholangiocarcinoma
Department of Health and Human Services enforce antikickback and self-referral laws that prohibit or limit certain conflicts of interest symptoms stomach cancer mentat ds syrup 100 ml online. Professional societies and associations of health care and educational institutions articulate norms and ethical standards for their members treatment bursitis buy mentat ds syrup 100 ml without prescription. Postings on institutional websites may be incomplete or not up to medications with gluten buy 100 ml mentat ds syrup with mastercard date, and some institutions choose not to reveal their policies. This chapter discusses ways in which these diverse supporting organizations can cooperate with and influence the academic and other institutions that have the primary responsibility for dealing with conflicts of interest in medical research, education, and practice. The chapter begins by considering some of the productive forms that support and cooperation can take. The discussion emphasizes the roles of collaboration, consensus building, and incentives in making conflict of interest policies more effective and compliance with them less burdensome. The chapter concludes with two recommendations that supplement the mostly mission-specific recommendations of earlier chapters. The first calls on supporting organizations to develop incentives for medical institutions to become more accountable for preventing, identifying, and managing conflicts of interest. The second calls for more research to provide a stronger evidence base for evaluating and improving conflict of interest policies. Such efforts seek to engage those affected by policies in the process of developing them to improve the policies. Supporting organizations may likewise be more successful if they engage research, educational, and other institutions in the process of designing incentives and setting standards and if they give those institutions some discretion on how to reach specific performance goals. The leaders of those institutions are often in the best position to identify barriers to accountability (including burdensome or confusing administrative procedures) and to suggest ways to overcome those barriers. They are also well situated to identify and reduce the unintended negative consequences of proposed policies or procedures. Some lessons for collaborative efforts that can be made to improve conflict of interest policies and practices are suggested by quality improvement initiatives within health care organizations. In this approach, the gathering and monitoring of outcomes data are crucial to identifying and reducing inappropriate variations in outcomes. In some cases, cross-institutional collaborations have helped institutions develop effective quality improvement programs. Some programs use transparency-the public reporting of organizational performance in relation to benchmarks-as a means of enhancing accountability and promoting competition to improve the quality of care. Accreditation agencies and voluntary groups have also encouraged this quality improvement process, and some universities have applied quality improvement models to university administration. The University of Wisconsin, for example, has an office of quality improvement that supports process improvement activities in administrative as well as academic areas, and its website showcases examples of activities that are potentially relevant for conflict of interest programs (University of Wisconsin, 2008). There are, of course, significant differences between quality improvement procedures and conflict of interest policies. Nonetheless, the mechanisms of collaboration, consensus building, and outcome measurement can usefully guide the relationships between outside supporting organizations and institutions directly involved in medical research, education, and practice. Some supporting organizations have been able to promote a consensus on important and often contentious aspects of conflict of interest policies. The parties included academic medical centers, teaching hospitals, industry, professional organizations, government agencies, and consumer groups. Over time, these and other initiatives have forged agreement on goals and recommendations regarding a number of controversial issues. Such collaborative consensus-building activities can address the practical concerns of individuals and institutions affected and make recommendations more credible and acceptable. Incentives Supporting organizations can devise incentives for institutions to adopt and implement conflict of interest policies. An example of an incentive for change in institutional policies and practices is the policy of the National Library of Medicine mentioned in Chapter 3. Just as the Medicare program and private health insurers have turned to pay-for-performance programs to provide incentives for quality improvement, so could insurance organizations offer incentives to institutions to adopt and maintain effective conflict of interest policies and to individuals to refrain from engaging in undesirable relationships with pharmaceutical, medical device, and biotechnology companies. For example, if preferred provider organizations publicly identified those participating physicians who agreed to decline gifts and marketing payments from industry, many physicians might decide that the benefits of being so identified outweigh the benefits of accepting such gifts and payments.
Diseases
- Poikilodermia alopecia retrognathism cleft palate
- Gastric dumping syndrome
- Auditory processing disorder
- Mental retardation microcephaly unusual facies
- Microcephaly glomerulonephritis Marfanoid habitus
- Lennox Gastaut syndrome
- Listeria infection
- Athetosis
- Proximal tubulopathy diabetes mellitus cerebellar ataxia
As a result symptoms yeast infection men cheap 100 ml mentat ds syrup with mastercard, there has been an increasing concern about the safety and health aspects of excessive exposure to symptoms xxy generic 100 ml mentat ds syrup with mastercard noise in daily operations symptoms restless leg syndrome mentat ds syrup 100 ml lowest price. Its purpose is to prevent the loss of hearing in military and civilian personnel who must work in hazardous noise environments. This is to be accomplished by a comprehensive program which includes noise exposure analyses, personal hearing protective devices, monitoring audiometry, education, and noise control engineering. In years past it was more or less accepted that a hearing loss accompanied certain jobs. This order requires the Navy to develop and implement programs to prevent any employee hearing loss arising from exposure to noise in the workplace. In many Audiograms devices are education is Navy and Marine Corps facilities, hearing conservation is being accomplished. The answer, though not simple, seems to lie with the perception of priorities and the 8-80 Otorhinolaryngology limits of resources. This chapter will discuss ways to implement a successful hearing conservation program. Appoint a responsible individual to coordinate all medical aspects of occupational noise control and hearing conservation. Assure identification and characterization of noise hazard areas within their purview according to paragraph two of enclosure (1). Assure that hearing conservation audiometry, clinical evaluation, and referrals are performed according to the standards of paragraph three of enclosure (1). Provide for earplug fitting support for military and civilian personnel within their program, according to paragraph four of enclosure (1). Assure certification or training, in accordance with enclosure (1) of this instruction, of Medical Department personnel, sound measurement equipment, audiometers, and hearing test booths involved in the hearing conservation program. Newly appointed coordinator, of hearing conservation programs should assess their resources and determine what deficiencies exist with their programs. They should determine: (1) If noise surveys have identified personnel exposed to hazardous noise and if so, have exposure risk assessments been performed, and: (2) Are required services such as hearing tests, fit- 8-81 U. This coordinator should ensure that adequately trained personnel are on board to provide services and that adequate audiometric facilities are available. Finally, the coordinator should represent the interests of hearing conservation at the command and staff level. It must be emphasized at all levels that there is no cure for noise-induced hearing loss, only prevention. No one is going to report automatically to the clinic and present themselves as a candidate for a program of hearing loss prevention. When individuals typically seek assistance, significant hearing loss has already occurred. Noise Measurement and Exposure Analysis the first step in the identification of noise-hazard areas and equipment, and noise-exposed personnel is the noise survey. The types of surveys and the different reasons for conducting a survey are discussed below. The preliminary survey may be any type of cursory or informal evaluation of possible noise hazards that any member of the hearing conservation team notices during walk-through of a work area. This could take the form of a response to a call from someone with a complaint of a noisy piece of equipment or noisy process. The rule-of-thumb criterion for this subjective appraisal is that a noise hazard may exist when it becomes necessary to raise your voice at a distance of three feet in order to communicate. The above may lead to a request for occupational health personnel to perform a noise survey. The survey should result in complete documentation of noise hazards and personnel at risk. An engineering noise analysis is performed when it is necessary to pinpoint noise sources for 8-82 Otorhinolaryngology noise control engineering. Control of noise at the source is the ultimate solution to prevent noiseinduced hearing loss. Specific documentation is required for A- weighted levels and listing of noise-exposed personnel where the noise levels are 84 dB(A) or greater. Noise survey information is also necessary when a civilian worker files a claim for compensation for hearing loss due to exposure to noise in the workplace. For military personnel, a noise exposure history should be available in every health record in order to verify that the hearing loss was due to occupational noise exposure rather than to some other factor.